
That is the question for Dr. Karatzios…
Dimitris Ilias
Take a look at the
featured Local Savings
at the bottom of this page!
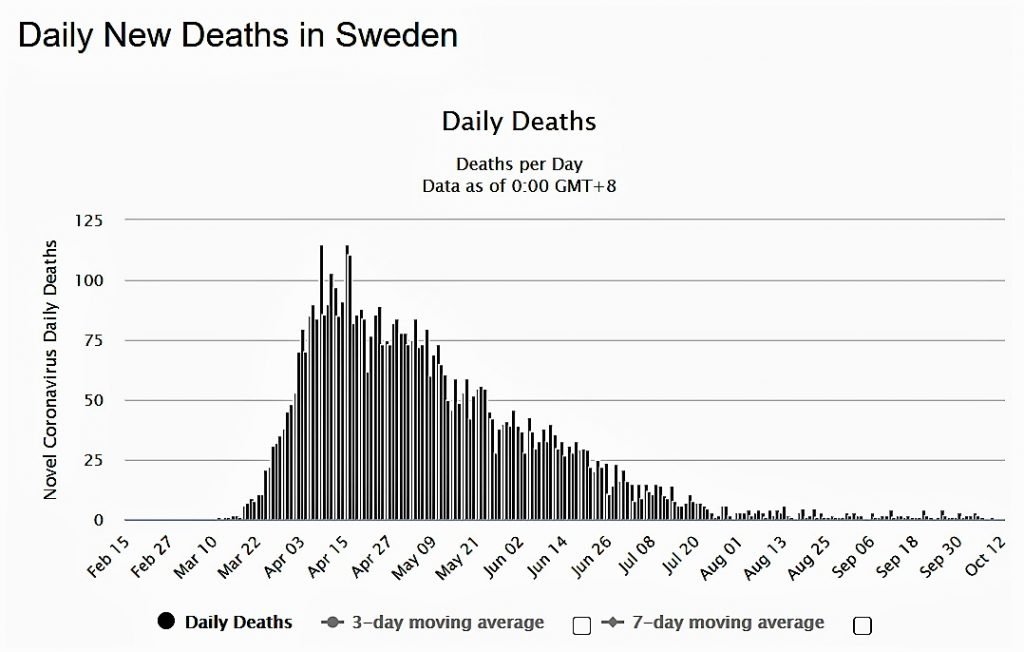
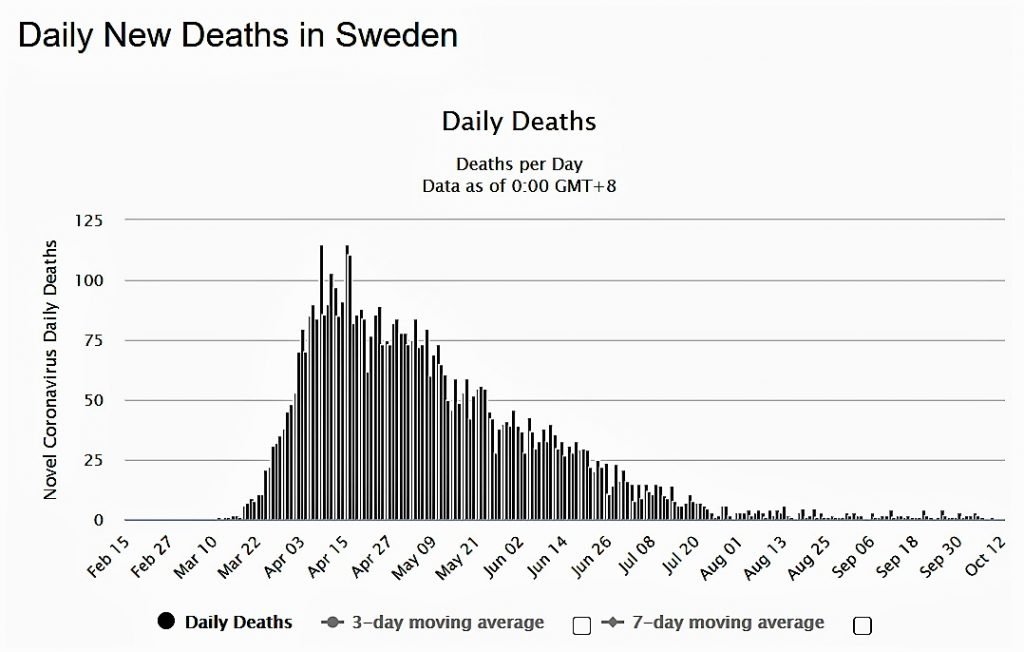
It was the great experiment! A country that went against all others in the way they handled Corona. They paid a price of almost 6000 dead Swedes. Their epidemiologists insisting against lockdowns and depending on the general good will of the population to follow the rules. The second wave appears to have arrived in Sweden as in all of the world, but according to the stats posted daily on Worldometers the daily cases are not as high as the spring and the deaths from the disease lately, up to now, have been infinitesimal (Graph A-Worldometers)
The WHO is also beginning change its story about the necessity of lockdowns and we are all left with the impression that this virus is toying with us, making our scientists change their diagnoses constantly.
So, where does the truth lie? Was Sweden right to sacrifice 6k of its citizens? We turned to our regular contributor Dr. Christos Karatzios assistant professor of Paediatrics/Infectious Diseases at the Montréal Children’s Hospital, to enlighten us about the Sweden situation.
Not convinced
In a previous articles Dr. Karatzios had critiqued their approach to lax mitigation strategies while all their neighbors and most countries on the planet closed down to “flatten the curve”.
According to the doctor, Sweden didn’t flatten any curve and while most deaths that occurred in that country were in the elderly and in nursing homes, it still is quite telling that their hospitals were overrun in the spring. They had to resort to refusing admissions to their ICUs to anyone over a certain age and (obese) weight or Body Mass Index.
When compared to similar countries in terms of population density and total population numbers, Sweden has one of the worst per capita death rates from COVID-19 in the world. Also, the excess mortality in Sweden between March and May 2020 has dwarfed that of its neighbors’.
Dr. Anders Tegnell (the controversial state epidemiologist responsible for the Swedish approach) admitted that Sweden did not achieve any form of “herd immunity” at the end of the first wave when reports of only 12% of Stockholm’s population had antibodies to SARS-CoV-2.
So it begs the question: what happened after the first wave? FB “epidemiologists and doctors” angrily denounced new mitigation strategies in the last few days here in Quebec, Canada.
Dr. Karatzio’s answer to them is: WAIT. We have all been humbled by this pandemic but what he has learned is this: leaders and countries that have boasted about getting control of the pandemic, have ended up eating their words more often than not.
Cases in Sweden have surged in the last 2 weeks and ever since people have returned to the largest urban centre Stockholm (home to 22% of Sweden’s population) after summer holidays (most Swedes leave for the sparsely populated countryside essentially socially distancing from others), and after schools started. Death surges usually lag by 2-4 weeks.
Sewer water analyses in the last month show high levels of SARS-CoV-2 in the water indicating widespread community infection.This is an indication that herd immunity has not been achieved and the Swedish idea may be just a dream. The WHO 🇺🇳 was too quick to state 2 weeks ago that the Swedish approach is a model “to study”. The Swedish model cannot be applied to other more densely populated countries of the world. Sweden is densely populated around Stockholm but essentially the hinterland is forest and tundra and sparsely inhabited. Stockholm was never spared and has not been spared.
The Swedish economy contracted just as much as other similar economies in locked countries. Maybe it fared a bit better in general but at a high cost to its people. Also, other countries with denser populations tried to emulate the Swedes and failed – locking down after the house caught fire – only to control the infections well into lockdown: the UK 🇬🇧, and the Netherlands 🇳🇱.
Countries that were caught off guard and didn’t have time to lock down before the house burned down had some of the worst death rates per capita: Italy 🇮🇹, Iran 🇮🇷, Spain 🇪🇸, France 🇫🇷, and Belgium 🇧🇪.
Countries that were caught off guard but locked down hard eventually controlled the infections: China 🇨🇳
Countries that saw the danger and locked down early and effectively, had a good first wave: Vietnam 🇻🇳, Thailand 🇹🇭, Taiwan 🇹🇼, Hong Kong 🇭🇰, Singapore 🇸🇬, Australia 🇦🇺, New Zealand 🇳🇿, Greece 🇬🇷, Finland 🇫🇮, India 🇮🇳, and Israel 🇮🇱.
Countries with inconsistent lockdowns or no lockdowns have some of the highest per capita death rates in the world: the US 🇺🇸, Brazil 🇧🇷, and Sweden 🇸🇪.
Countries that initially did well and opened up too fast or recklessly are now seeing big surges and the deaths have started to climb: Israel 🇮🇱, Greece 🇬🇷, Canada 🇨🇦, and India 🇮🇳. As a result, new mitigation measures ranging from semi to full lockdowns have been reimplemented.
Conclusions according to Dr. Karatzios


It is too soon to make any conclusions but the numbers are not looking rosy for Sweden as it is entering its second wave.
The Swedish model cannot be used as an example of a success story. Too many people have died, the economy isn’t significantly better than other places, and herd immunity has not been achieved.
The Swedish people have paid a high price for this.
Sweden has started mitigation strategies and has admitted it may need to close down some sectors and even Stockholm if cases continue to rise sharply. They didn’t test and contact trace as much before. They are starting now.
Lockdowns (full or semi with effective testing and case tracing) work. No one likes them but there is no sugar coating this.
The Swedish story is not over and the Dr. Karatzios would be curious to see how it unfolds. He has reservations about success (and always had) looking at reports out of Sweden.
Stool PCR testing
Stool PCR testing for the SARS-CoV-2 has been used as an early warning of an upcoming surge in cases. The ability to detect SARS-CoV-2 in the upper respiratory tract ceases after 2 to 3 weeks post-symptom-onset in most patients. In contrast, SARS-CoV-2 can be detected in the stool of some patients for greater than 4 weeks, suggesting that stool may hold utility as an additional source for diagnosis.
The graph below shows how the rise in detection of SARS-CoV-2 in sewer water precedes the wave of positive cases.
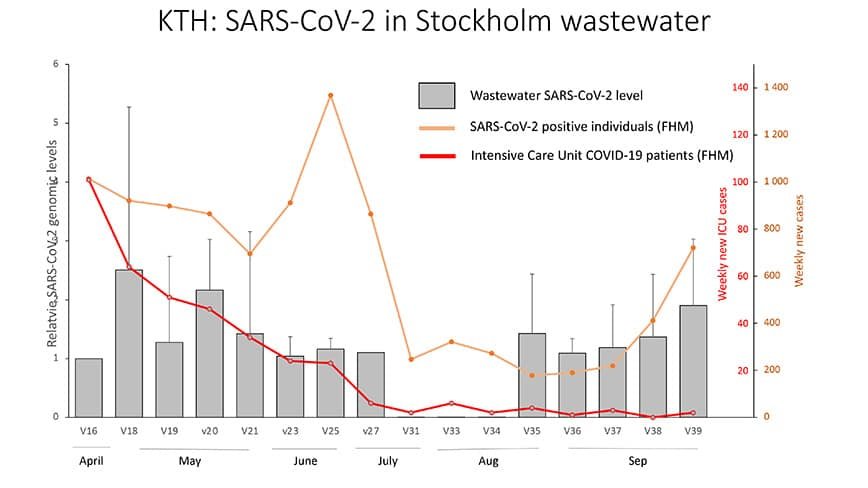
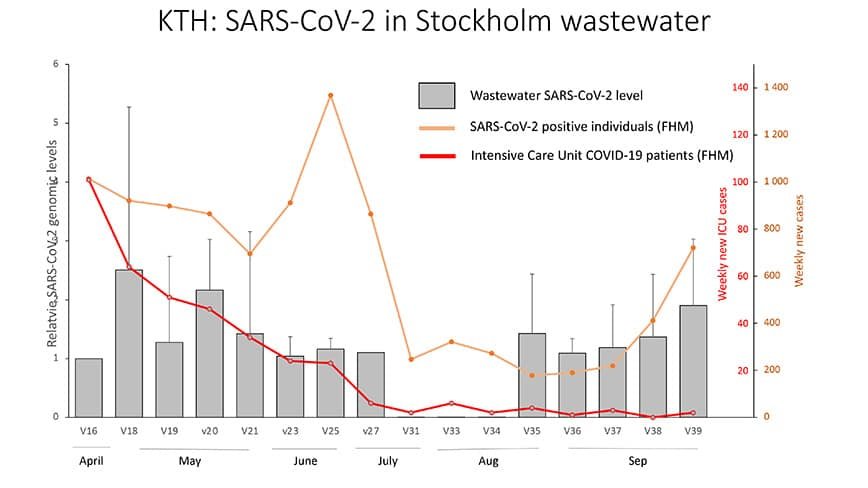
Dr. Karatzios has posted about PCR detection in sewage as an early warning tool Public Health can use to gauge an upcoming surge and take the necessary measures to prevent a wave.















